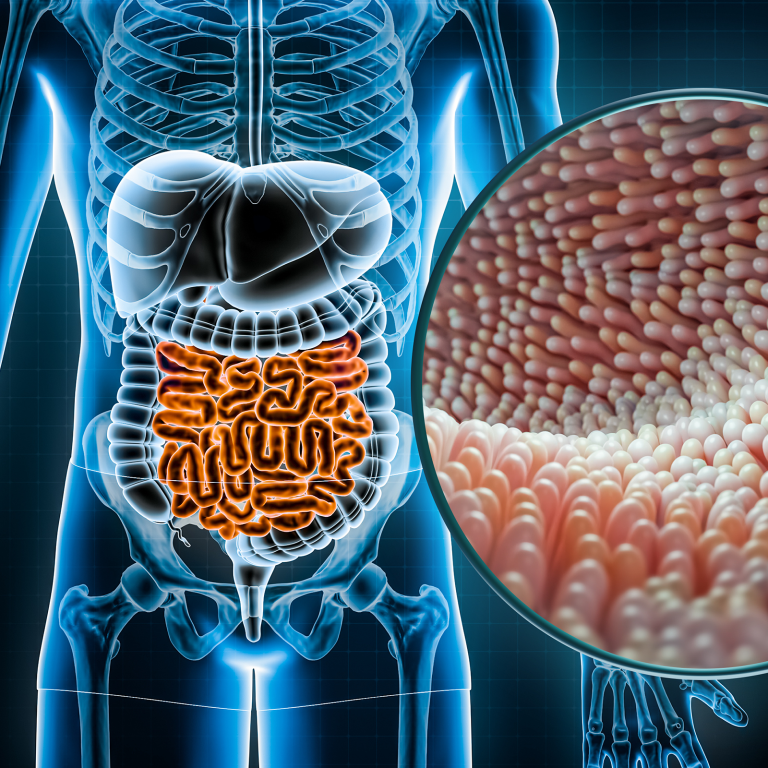
Endometriosis is a painful, inflammatory condition that affects one in 10 Australian women of reproductive age. Despite being a common disorder, it takes most women an average of eight years to receive a diagnosis. Unsurprisingly, the internet is packed with alternative therapies for treating the condition, but are any of them helpful and can a gluten-free diet help? CARA BOATSWAIN investigates.
What is endometriosis?
“Endometriosis occurs when endometrial tissue, which is normally found within the uterus, is displaced in other areas of the body,” explains nutritionist and natural fertility specialist Tasha. . .