Lifelong adherence to a gluten-free diet is the only treatment for coeliac disease. Dietitian, LORI WELSTEAD from the University of Chicago Celiac Disease Centre shares with us her tips on how to follow a gluten-free diet, that’s good for you too.
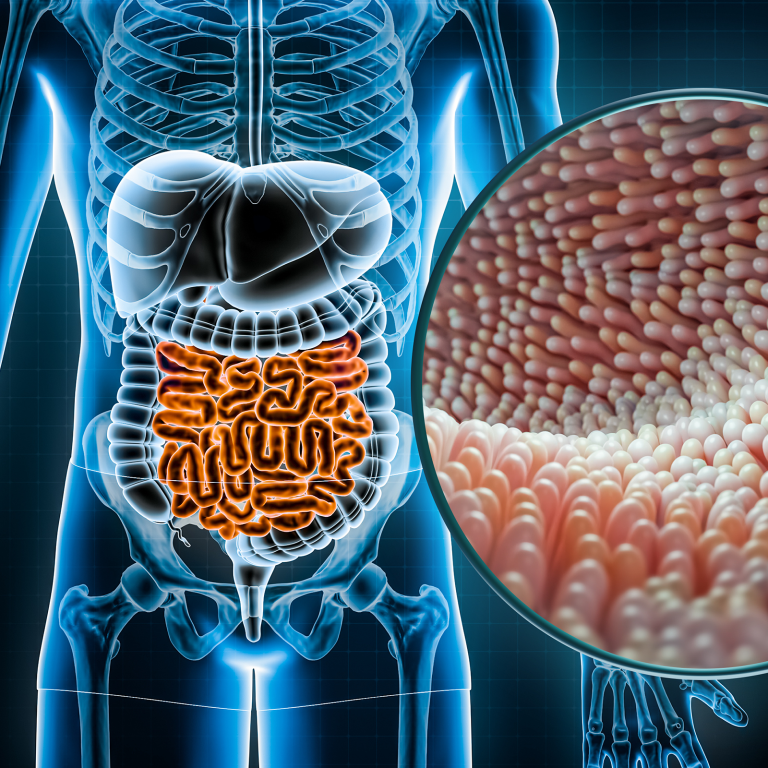
Currently, the only treatment for coeliac disease is a life-long avoidance of gluten-containing foods. Strict adherence to the gluten-free diet often minimises bloating, diarrhoea, weight loss, fatigue and begins the healing process. I have known patients who have begun to feel improvements. . .